EHMA 2021 Conference Programme
Check out our programme of events below:
Day 1 – Wednesday, 15 September 2021
 Health Management: managing the present and shaping the future
Health Management: managing the present and shaping the future
The EHMA Conference is the preeminent place to share experiences, skills, and competencies in the field of health management through interactive workshops, scientific presentations, and engaging debates.
Bringing practitioners, researchers, policymakers, and academics together to share solutions has never been more important than today. As European health systems are dealing with current challenges and planning their readiness for the future, health management will be at the center of providing solutions for these unprecedented difficulties.
Opening ceremony
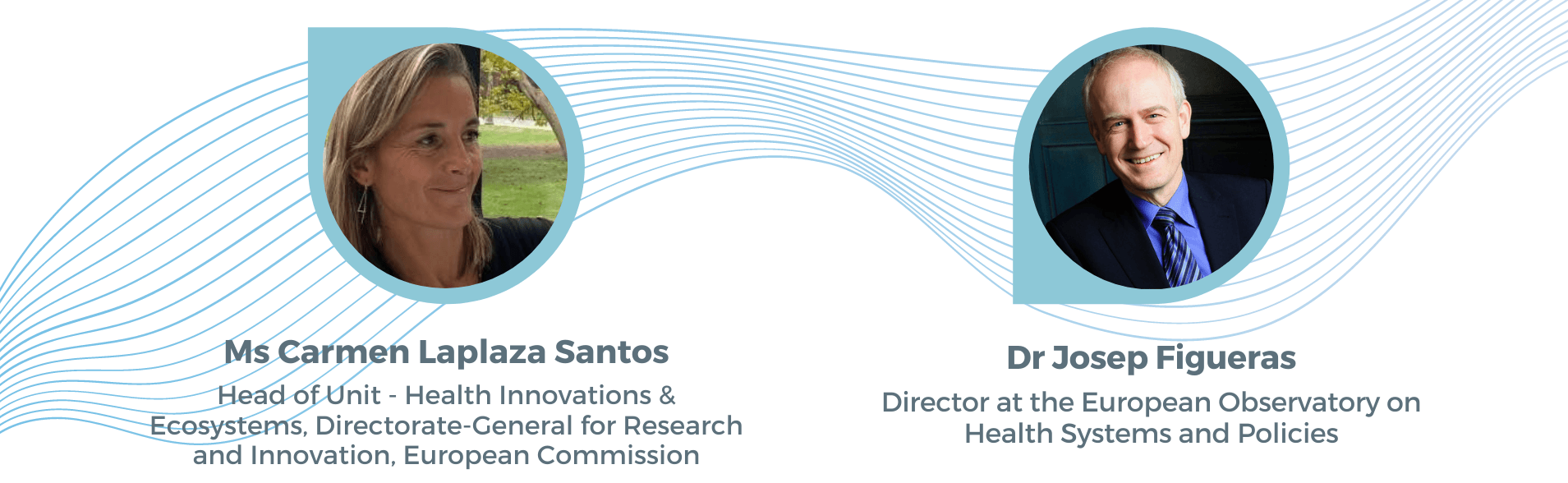
Institutional greetings by
- Dr Axel Kaehne, President, European Health Management Association (EHMA)
- Prof José Fragata, Vice-Rector of Universidade NOVA de Lisboa
Opening addresses by:
- Ms Carmen Laplaza Santos, Head of Unit – Health Innovations & Ecosystems, Directorate-General for Research and Innovation (DG RTD), European Commission
- Dr Josep Figueras, Director, European Observatory on Health Systems and Policies
Moderated by Dr Alexandre Lourenço, President, Associação Portuguesa de Administradores Hospitalares (APAH) and Master of Ceremonies of EHMA 2021
Connect with participants and explore the exhibition area
 Shaping health systems for a post-COVID world
Shaping health systems for a post-COVID world
Over the last year, national health systems and European and international health organisations have worked tirelessly to deliver emergency services, while confronting challenges such as hospital capacity and workforce planning. As health systems are progressing towards managing the pandemic and creating their recovery plans, they are also thinking about how to strengthen the resilience and sustainability of their resources in an ever-changing context.
What are the lessons learnt from COVID-19 about managing resilient and flexible healthcare systems? What are the medium and long-term effects of COVID-19 on European health systems? How can health systems and services organise and adapt for a post-COVID context? What are the best practices to shape health systems for the recovery period?
Keynote:
- Dr Hans Kluge, Regional Director for Europe, World Health Organization (WHO) (recorded message)
Speakers:
- Prof Maurizio Cecconi, President, European Society of Intensive Care Medicine
- Ms Adelina Comas-Herrera, Assistant Professorial Research Fellow, Care Policy and Evaluation Centre (CPEC), London School of Economics; Curator, LTCcovid.org
- Dr Ellen Kuhlmann, President, EUPHA section on Health Workforce Research; Senior Researcher, Hannover Medical School
Moderated by Dr Alexandre Lourenço, President, Associação Portuguesa de Administradores Hospitalares (APAH) and Master of Ceremonies of EHMA 2021

Connect with participants and explore the exhibition area
 POSTER PRESENTATIONS
POSTER PRESENTATIONS
In this pitching session authors will present their posters. Posters will remain available in the exhibition area for the entire duration of the Conference. You can contact the authors via the Conference platform for any questions or more information.
In this session the following posters will be presented:
Under the sub-theme ‘Managing the digital transformation’
- Digital technologies in healthcare: what best practices and challenges? by Dr Antonio Fusco
- Digital primary care visits designed for different patient segments – a systematic review by Ms Sanna Lakoma
- Artificial Intelligence innovations in a small medical practice: perspectives and obstacles by Ms Anna Wohlthat
- How did COVID–19 pandemic help implement telemedicine in health systems? Short overview of facilitators and barriers by Ass. Prof Dr Eva Turk
Under the sub-theme ‘Health workforce’
- Occupational risk perception and work-related diseases prevention by Ms Paula Madaleno
- Occupational risk perception in health education and research: better knowledge, better prevention by Ms Paula Madaleno
- Health workforce support needs in the light of COVID crisis (example from Serbia) by Prof Marija Jetvic
- Metrological assessment of infusion pump emergency practice in times of pandemic: The COVID-19 case by Dr Vania Silverio
 Towards personalised medicine – an innovative diagnostic tool to identify cardiovascular complications in COVID-19 patients
Towards personalised medicine – an innovative diagnostic tool to identify cardiovascular complications in COVID-19 patients
This session will examine the benefits of personalised disease management on health systems and discuss how patient-centered care and personalised medicine can improve disease outcome and enhance patients’ quality of life. Cardiovascular complications arising from COVID-19 are known to contribute significantly to mortality rates. The COVIRNA project aims to improve individualised surveillance, care and follow-up of COVID-19 patients by identifying those who are at risk of developing fatal cardiovascular complications.
This session will also cover additional questions that a crucial to consider when moving towards personalised medicine: how do we bring innovations, such as the COVIRNA tool, to patients? How can AI be employed to develop predictive models? And what are the challenges associated with sharing data across health institutions?
Speakers:
- Dr Yvan Devaux, Head of the Cardiovascular Research Unit at Luxembourg Institute of Health (LIH)
- Dr Vincent Mooser, Canada Excellence Research Chair in Genomic Medicine; Director Québec COVID-19 Biobank; Professor, Department of Human Genetics, Faculty of Medicine, McGill University, Canada
- Dr Kanita Karaduzovic-Hadziabdic, Assistant Professor, International University of Sarajevo
- Mr. Venkata Satagopam, Deputy Head at Bioinformatics core, Luxembourg Centre For Systems Biomedicine (LCSB), University of Luxembourg
- Dr Eric Schordan, Chief Scientific Officer Biomarker R&D at Firalis Molecular Precision
Moderated by Ms Adriana Voicu, Project Manager, Cardiovascular Research Unit, Luxembourg Institute of Health (LIH)
This session is hosted by the COVIRNA project. COVIRNA is a patient-centred Innovation Action aiming to generate a diagnostic tool to identify COVID-19 patients at risk of developing fatal cardiovascular complications. This project has received funding from the European Union’s Horizon 2020 Research and Innovation Programme under grant agreement No 101016072
 ABSTRACT SESSION on Healthcare policies
ABSTRACT SESSION on Healthcare policies
Well-designed, evidence-based, and result-driven healthcare policies can reduce health inequalities, support the provision of safe and high-quality patient care, and ensure the efficient use of resources, thus leading to improvements in population health. This abstract session will explore the effects of healthcare policies on the provision and quality of care in various countries across the globe.
The following abstracts will be presented:
- National strategies and programmes: a multisectoral approach in supporting public health at municipal level in Serbia
Prof Milena Vasic, Institute of Public Health of Serbia, Serbia; Faculty of Dentistry, Serbia - Cultural implications on global medicine and health policy reform: a comparative analysis of Japan and United States of America
Ms Kendra Pyne, University College London, United Kingdom - Modelling peer review as a means of regulatory compliance in specialised commissioned services in the NHS
Dr Axel Kaehne, Edge Hill University, United Kingdom - The efficacy of a Dutch governmental support program for quality improvement in nursing homes
Dr Paulien Vermunt, Vilans, Centre of Expertise for Long-Term Care, The Netherlands
Moderated by Prof. Alexandre Abrantes, Escola Nacional de Saude Publica, Portugal
 ABSTRACT SESSION on Improving access to healthcare
ABSTRACT SESSION on Improving access to healthcare
Facilitating access to healthcare implies improving the affordability, accessibility, acceptability, availability, and adequacy of care services. As highlighted by this abstract session, many subgroups of the population still face considerable barriers that impede them from accessing the necessary healthcare resources.
The following abstracts will be presented:
- Assessing the impact of anti PD-1/PD-L1 inhibitors on Cancer Care Health and Budget in Ireland
Dr Iseult Browne, Mater Misericordiae University Hospital, Ireland - Delivering value and improving care with primary care estate
Mr Chris Santer, Primary Health Properties (PHP), United Kingdom - Migrants’ access to health care services: A cross-sectional study in Portugal
Dr Ana Gama, Escola Nacional de Saúde Pública da Universidade NOVA de Lisboa, Portugal - 10 years after: Knowledge of diabetic patients in Slovenia
Ass Prof Dr Eva Turk, University of Oslo, Norway; University of Maribor, Slovenia - Defending the rights of children with special needs
Dr Kinga Zdunek, Public Health Department, Medical University of Lublin, Poland
Moderated by Prof Sílvia Lopes, Assistant Professor, Escola Nacional de Saúde Pública da Universidade NOVA de Lisboa, Portugal
 ABSTRACT SESSION on Managing the digital transformation
ABSTRACT SESSION on Managing the digital transformation
The use of digital technologies in the healthcare sector has been increasing in the past years, and the onset of the COVID-19 pandemic has further highlighted the need for digital solutions. Digital health has the potential to make health systems more responsive, resilient and sustainable. Moreover, telemedicine can help ensure continuity of care and facilitate the management of chronic conditions. Digital transformation in healthcare is thus key to achieve high-quality patient care.
The following abstracts will be presented:
- Implementation and transfer of successful digitally enabled integrated person-centred care solutions across Europe – The JADECARE Joint Action
Mr Jon Txarramendieta, Kronikgune Institute for Health Services Research, Basque Country, Spain - SIDERA^b, a new telerehabilitation approach: economic and organisational impacts
Dr Daniele Bellavia, Centre for Health Economics, Social and Health Care Management, Carlo Cattaneo – LIUC University, Italy - Acceptability of digital technologies: the intention to adopt T-CUBE solution in COVID-19 pandemic
Dr Lucrezia Ferrario, Centre for Health Economics, Social and Health Care Management, Carlo Cattaneo – LIUC University, Italy - Effectiveness of indicators for national control (KUVA indicators) as a decision-making tool
Ms Petra Kokko, Finnish Institute for Health and Welfare (THL), Finland - Socio-organisational evaluation of a tele-expertise experiment for skin cancer detection: the perspective of General Practitioners
Dr Clarissa Seixas, Ecole de Hautes Études en Santé Publique, France; Universidade do Estado do Rio de Janeiro, Brazil - A national survey on the knowledge and perception of artificial intelligence in radiology
Dr Ivo Dumic-Cule, Childrens Hospital Srebrnjak, Croatia
Moderated by Prof. Teresa Magalhaes, Escola Nacional de Saude Publica, Portugal
Connect with participants and explore the exhibition area
Harnessing the experience of the COVID-19 pandemic to enable and accelerate Digital Health Transformation
While digital health has been identified and advocated for as a facilitator to improve access to, provision and quality of health care, contributing to universal health coverage (UHC), its actual implementation and uptake in practice have been slow in many European countries. The potential of digital health is not being fully utilised so far, for improving person-centred health care, strengthening health research and building better and more resilient health systems.
The COVID-19 pandemic has brought rapid and unprecedented changes in the area of digital health; a multitude of innovative, pragmatic digital solutions have been developed and successfully used to mitigate the effects of COVID-19, both in responding directly to this public health emergency and indirectly for maintaining essential health services. However, digital health plans, strategies, policies and actual implementation were not always coherent across countries in the European region throughout the pandemic, leaving space for improvement through cross-country learning and better collaboration. The COVID-19 pandemic has proven to be an opportunity for digital health to excel widely across the European region; whether this will permanently change the provision of health care is yet to be seen.
This session will
- provide a framework for understanding digital health within the general context of innovation and highlight the main areas of activity during the COVID-19 pandemic across European countries as well as barriers and facilitators for its uptake before and during the pandemic, drawing from the latest policy brief of the European Observatory on Health Systems and Policies.
- present a summary of the lessons distilled during the 2021 edition of the Observatory´s Venice Summer School, which explored the potential of digital health to provide data for policy and practice, transform the provision of health care and fuel research, and strategies to sustain new digital health solutions post-pandemic.
- highlight the main tenets for the development of the World Health Organization’s global digital health strategy.
- allow for participant interaction and exchanging views to build on existing insights and further cross-country learning.
Speakers:
- Dr Gemma Williams, Research Fellow, European Observatory on Health Systems and Policies
- Dr Florian Tille, Technical Officer, European Observatory on Health Systems and Policies
- Prof. Fidella Cascini, Assistant Professor at the Department of Hygiene and Public Health at Università Cattolica del Sacro Cuore, (Italy)
Moderated by Dr Dimitra Panteli, Programme Manager, European Observatory on Health Systems and Policies
This session is hosted by the European Observatory on Health Systems and Policies. The Observatory is a partnership that brings together different policy perspectives to identify what health systems and policies evidence Europe’s decision makers need. The Observatory then generates and shares the evidence in print, in ‘person’ and on-line – acting as a knowledge broker and bridging the gap between academia and practice.
 Winter is coming: the burden of Respiratory Syncytial Virus (RSV) on health systems in Europe
Winter is coming: the burden of Respiratory Syncytial Virus (RSV) on health systems in Europe
Respiratory Syncytial Virus (RSV) is a leading cause of acute low respiratory tract infections in children, and a major contributor of the winter pressures that burden healthcare organisations in Europe every year. In order to determine the effects of RSV on European healthcare systems and facilitate evidence-based decision making on RSV treatment and prevention, it is important to document the burden of RSV on the healthcare system and characterise its effects across the care setting.
This session begins with EHMA’s ongoing survey on the burden of RSV on health systems in Europe. Topics of discussion include: the system-wide pressures that affect health system performance in the peak RSV season; current practices for the treatment and management of RSV in the community and hospital care; and the optimal approaches and strategies required to manage RSV infection management in the community.
Setting the scene:
Dr Christian Felter, RSV Franchise Medical Head, Sanofi Pasteur
Keynote:
Prof Javier Díez-Domingo, Head of the Vaccine Research Department, Centre of Public Health Research of Valencia-FISABIO, Spain
Panel discussion:
- Dr Călin Bumbuluț, Senior Family Physician – Satu Mare Family Physicians Association, Romania; President, European Union of General Practitioners (UEMO)
- Prof Susanna Esposito, Director of Specialization School in Pediatrics, Department of Medicine and Surgery, University of Parma, Italy
- Dr Simon Nadel, Imperial College Healthcare NHS Trust, UK
- Dr Fransisco Mourão, Treasurer, European Junior Doctors
Moderated by Mr George Valiotis, Executive Director, EHMA
This session is hosted by Sanofi Pasteur. Respiratory Syncytial Virus (RSV) is a common, contagious seasonal pathogen that will infect nearly all babies by their second birthdays. RSV is a leading cause of lower respiratory tract infection, mainly bronchiolitis and pneumonia, in infants and young children, resulting in annual epidemics worldwide. Sanofi has partnered with AstraZeneca to double down on the two companies’ commitments to finally help bring RSV, a pervasive and life-threatening infection for very young children, under control in the future.
Connect with participants and explore the exhibition area
 ABSTRACT SESSION on Health workforce
ABSTRACT SESSION on Health workforce
The availability and quality of the health and care workforce is key for effective health system performance. To deliver safe healthcare, health and care workforces must be adequately supported, protected, and equipped. This includes not only adapted Personal Protective Equipment during the COVID-19 pandemic and beyond, but also psychological safety and resilience training. In addition, the shortage of health workforce is of critical concern and one way to face the problem is through task shifting.
The following abstracts will be presented:
- Examining psychological safety in healthcare teams to inform the development of interventions: combining observational, survey and interview data
Ms Róisín O’Donovan, UCD Centre for Interdisciplinary Research, Education and Innovation in Health Systems (UCD IRIS) | School of Nursing, Midwifery & Health Systems, Ireland - Evolution of tasks and responsibilities at home care level: a focus on nursing role
Dr Maria Picco, Politecnico di Milano, School of Management, Italy - Exploring the mediating role of use of performance feedback in the feedback orientation-performance relationship in healthcare
Ass Prof Marco Giovanni Rizzo, Università Cattolica del Sacro Cuore, Italy - Ready for lunch? Bread and butter of care integration
Dr Nour Alrabie, U Amsterdam, The Netherlands; Queen’s University, United Kingdom - Mapping mental health professionals’ journey along the Digital Mental Health intervention process: a qualitative study
MsC Cristina Mendes-Santos, Linköping University, Sweden; NOVA National School of Public Health, Portugal; Fraunhofer Portugal AICOS, Portugal
Moderated by Ms Laura Cande, Projects & Policy Consultant, EHMA
 ABSTRACT SESSION on Person-centered care
ABSTRACT SESSION on Person-centered care
Person-centered care puts the patient at the center of decision-making, and involves the patient in the planning, developing, and monitoring of care to ensure that their needs are met. As will be made evident during this session, person-centered care can be achieved through various approaches, including active participation of patients in goal setting, social prescribing, and shared decision-making concerning resource allocation.
The following abstracts will be presented:
- Positioning Social Prescribing in the scenario of community-based interventions for the transformation of mental health services for children, adolescents and young people: a review
Ms Isabel Farina, Management Engineering Department, Politecnico di Milano, Italy - Gender as a driver of healthcare sustainability: a systematic literature review
Dr Francesca Donofrio, University of Bari Aldo Moro, Italy - Public perspectives on using societal values in oral healthcare decisions
Ms Bronagh McGuckin, Newcastle University, United Kingdom - Breast cancer patients’ attitudes toward Digital Mental Health
MsC Cristina Mendes-Santos, Linköping University, Sweden; NOVA National School of Public Health, Portugal; Fraunhofer Portugal AICOS, Portugal
Moderated by Prof Sónia Dias, Escola Nacional de Saude Publica, Portugal
 ABSTRACT SESSION on Health management and COVID-19
ABSTRACT SESSION on Health management and COVID-19
The COVID-19 pandemic has created numerous managerial and operational challenges surrounding the delivery of healthcare. Faced with equipment and workforce shortages, reduced capacity, and financial losses, health managers were forced to radically transform their organisations and redesign their care models to deal with the unprecedent patient influx and meet the extraordinary demand for healthcare.
The following abstracts will be presented:
- Direct costs of COVID-19 inpatient admissions at a University Tertiary Care Centre
MSc Joana Seringa, Centro Hospitalar Universitário de Lisboa Central, E.P.E., Portugal; NOVA National School of Public Health, Universidade NOVA Lisboa, Portugal - Health management and governance – An excursion on leadership in the wake of the pandemic in the case of alpine winter tourism 2020 in Tyrol and Vorarlberg
MA, BA Lukas Kerschbaumer, Management Center Innsbruck, The Entrepreneurial School, Austria - Response to COVID-19 in France: identify the critical success factors of patient inter-regional transfers
Dr Anne Girault, EHESP, France - Partnership-working in health and social care: A multi-national, regional analysis of the impact of COVID-19 on health and social care integration
Dr Jessica Lubin, Researcher, Good Governance Institute; Dr Abigail Menke, Saint Louis University – Heartland Center for Population Health and Community Systems Development; Dr Sofie Van Steendam, Master student Healthcare Management and Policy, KU Leuven.
- Pillars for planning a COVID-19 Mass Vaccination Center: the Novegro, Milan experience
Dr Giovanni Gaetti, Sovraintendenza Sanitaria, Gruppo San Donato, Italy - Managing Health Systems Better: Lessons learned from COVID-19 in the Anglophone Caribbean
Prof Damian Greaves, Professor at the Department of Humanities and Social Sciences at St. George’s University
Moderated by Prof. Julian Perelman, Escola Nacional de Sude Publica, Portugal
How to implement value-based healthcare projects – two different approaches!
Speakers:
- Dr Florian Ruter, Head, Quality Management, University Hospital Basel, Switzerland
- Dr Marta Soares, Portuguese Oncology Institute of Porto (IPO Porto), Portugal
Moderated by Dr Alexandre Lourenço, President, Associação Portuguesa de Administradores Hospitalares (APAH).
This session is hosted by Roche. Committed to improving lives since the company was founded in 1896 in Basel, Switzerland, today Roche creates innovative medicines and diagnostic tests that help millions of patients globally. Roche was one of the first companies to bring targeted treatments to patients. With combined strength in pharmaceuticals and diagnostics, Roche has been at the forefront of personalised healthcare.

Day 2 – Thursday, 16 September 2021
 PhD Session
PhD Session
This session will feature presentations of the 6 shortlisted abstracts that are competing for the Karolinska Medical Management Centre (MMC) & EHMA Research Award, an annual award for the best contribution associated with a doctoral thesis related to health management.
- Through the physician’s lens. A micro-level perspective on the structural adaptation of professional work
Miss Rachel Gifford, University of Groningen, The Netherlands - A systems theory approach on analysing the cost-effectiveness of public care provision systems
Mr Olli Halminen, HEMA Institute, Department of Industrial Engineering and Management, Aalto University, Finland - ‘It’s always about the child’: exploring the moral actions of Irish pediatric nurses and doctors in response to moral conflicts in their practice – a Critical Incident Technique study
Dr Carol Hilliard, Children’s Health Ireland at Crumlin, Ireland - Impact of co-production on satisfaction in healthcare sector: an analysis from the patients’ perspective
Mr Simone Laratro, Università Cattolica del Sacro Cuore, Italy - Implementing change within healthcare teams: a qualitative study exploring the influence of context on implementation success
Dr Lisa Rogers, University College Dublin Centre for Interdisciplinary Research, Education, and Innovation in Health Systems (UCD IRIS), University College Dublin School of Nursing, Midwifery and Health Systems, Ireland - Getting married or living-apart-together? Healthcare executives’ perspectives on the pros and cons of mergers and collaborations
Wouter van der Schors, Erasmus University Rotterdam, The Netherlands
Moderated by Dr Pamela Mazzoccato, Associate Professor of Medical Management at Karolinska Institutet, Sweden & Director of Research & Development, Education and Innovation at Södertälje Hospital, Sweden
This award is supported by the Karolinska Medical Management Centre (MMC). MMC offers academic education to healthcare professionals and managers, and carry out research to support a science-based management practice in health care. Their vision is to address how resources in the form of competence, knowledge, material and other assets can best be used and developed to improve human health. Their aim is to develop new knowledge through interaction with our partners and fruitful meetings between theory and practice.
 ABSTRACT SESSION on Value-based healthcare
ABSTRACT SESSION on Value-based healthcare
In the past years, health systems started shifting towards Value-Based Health Care (VBHC) in an intent to move away from volume-driven care. Value-based healthcare focuses primarily on improving patient health outcomes, thus creating more value for patients. In addition, value-based healthcare controls the costs of care by discouraging overtreatment and waste of resources.
The following abstracts will be presented:
- The implementation of Value-Based Healthcare (VBHC): a scoping review
Ms Dorine van Staalduinen, Leiden University Medical Center, The Netherlands - Clinical Costing as a cost-component of Value-Based Healthcare: a systematic literature review
Ms Grazia Dicuonzo, Senior Lecturer of Business Administration, University of Bari Aldo Moro, Italy - Implementing value-based health care at the provider level: critical decision areas and related contextual factors
Dr Mandar Dabhilkar, Stockholm University, Sweden
Moderated by Prof. Tiago Rua, Escola Nacional de Saude Publica, Portugal
 ABSTRACT SESSION on Continuity of hospital care
ABSTRACT SESSION on Continuity of hospital care
Continuity of care is achieved through the coordination and integration of care across sectors, healthcare settings, providers and users. Continuity has shown to enhance treatment adherence and outcomes, result in higher patient and provider satisfaction, and improve patients’ quality of life. The COVID-19 pandemic seriously hampered continuity of care due to closure of primary care practices, postponed appointments, shortages of medicine, and disruption of patient-provider interactions.
The following abstracts will be presented:
- Establishment of a hospital-territory computer network for the management and care of patients in “pediatric palliative care” in Umbria
Dr Fabrizio Ruffini, Azienda Ospedaliera di Perugia, Italy - Determinants of hospital delayed discharges in Portugal
Dr Alexandre Lourenço, Nova School of Business & Economics, Universidade NOVA de Lisboa, Portugal; Centro Hospitalar e Universitário de Coimbra, Portugal; National School of Public Health, Universidade NOVA de Lisboa, Portugal - The Occupational Therapist and the discharge support intervention program
Prof Maria de Guadalupe Comparada Almeida, Instituto Politécnico de Beja, Portugal - Hospital-at-home – challenge in surgical pathology
Dr Miranda Rute, Clinical Pharmacist
Moderated by Prof. Paulo Boto, Escola Nacional de Saude Publica, Portugal
 EHMA PIE: Improving healthcare access and outcomes
EHMA PIE: Improving healthcare access and outcomes
EHMA PIE is a space for discussions that are Provocative, Innovative and
Encouraging (PIE) and can help shape the future of health management. Through EHMA PIE, we aim to address complex topics, spark provocative discussions, and foster connections across the entire health ecosystem.
The following ideas will be presented:
- Impact of healthcare funding on patient outcomes
Mr. João Frutuoso, Hospital Vila Franca de Xira, Clinical practice (M.D.) and Union Delegate - Moving beyond RCTs: Tapping the potential of Real-World Data for advancing clinical research and improving post-treatment in breast cancer
Dr Ioannis Sarafis, Postdoctoral Researcher, Aristotle University of Thessaloniki
Moderated by Dr Elly Breedveld, Director, Stichting Perspekt, and Board Member, EHMA
Connect with participants and explore the exhibition area
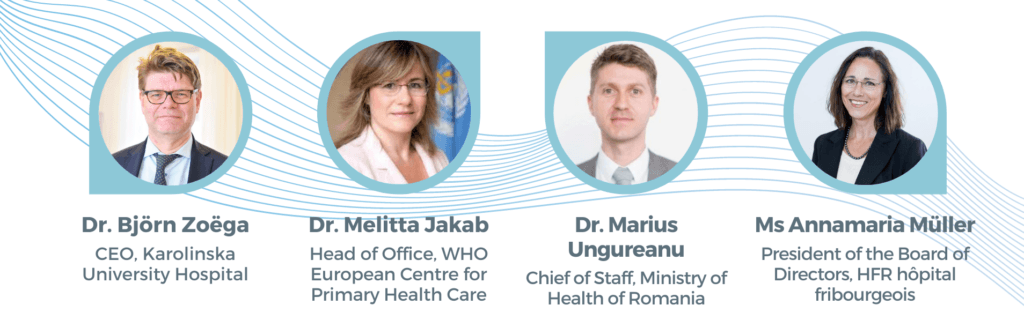
 Leadership for the future of healthcare
Leadership for the future of healthcare
In the past year, the role of health leadership has been in the spotlight as the effect of health leaders’ decisions has been observed and scrutinised. With the increasing demands on health services, rapidly changing context, and the adoption of technological innovations, health systems and organisations are having to revisit and adapt their leadership styles and strategies.
How are changes in healthcare impacting leadership? How to improve management and leadership in healthcare? How to engage clinicians as servant leaders for the organisation? How can health care leaders participate in preparing for the health systems of the future?
Setting the scene:
Ms Izabela Grape, Representative, Breast Cancer Society Amazona
Speakers:
- Dr Melitta Jakab, Head of Office, WHO European Centre for Primary Health Care
- Ms Annamaria Müller, President of the Board of Directors, HFR hôpital fribourgeois
- Dr Marius Ungureanu, Chief of Staff of the Minister of Health of Romania
- Dr Björn Zoëga, CEO, Karolinska University Hospital
Moderated by Dr Alexandre Lourenço, President, Associação Portuguesa de Administradores Hospitalares (APAH) and Master of Ceremonies of EHMA 2021
Connect with participants and explore the exhibition area
 POSTER PRESENTATIONS
POSTER PRESENTATIONS
In this pitching session authors will present their posters. Posters will remain available in the exhibition area for the entire duration of the Conference. You can contact the authors via the Conference platform for any questions or more information.
In this session the following posters will be presented:
Under the sub-theme ‘Governance and Leadership’
- E-handover in surgery improves clinical efficiency and adherence to COVID-19 infection control measures by Dr Neville Jacob
- Quality improvement plans in Allied Air and Space Commands – A case study from the NATO STEADFAST JUPITER-JACKAL 2020 exercise by Dr Jacopo Frassini
- Developing synergy across transdisciplinary and through multisectoral approaches within the context of Transformational Change in the Kingdom of Saudi Arabia through Collective Leadership by Dr Safa Alakhdhair
- Structural registration and discussion of patient outcome data for improving quality of cardiac care: approach of the Netherlands Heart Registration by Dr Niki Medendorp
- Assurance: a key steering tool for good leadership by Mr Joao Figueiredo
- Organisational impact related to the introduction of automated technologies for pharmaceutical logistics in the hospital setting by Dr Daniele Bellavia
- Proposals for financial stability and structural reform of the Croatian healthcare system by Dr Dražen Jurković
- Governance and organisation of Academic Medical Centers – challenges in a changing landscape by Ms Ester Cardinaal
- The role of procurement in driving innovation and delivering better outcomes by Ms Gaynor Whyles
 Governance for healthcare transformation: harnessing the power of laboratories
Governance for healthcare transformation: harnessing the power of laboratories
Laboratories have the potential to favourably impact decision-making and clinical governance as powerful collaborators and catalysts of value to health systems. Well beyond their contribution to medical diagnosis and therapy, laboratory insights guide the development of precision and personalised medicine, prompt the shift towards prevention, and are protagonists for innovation and transformation.
By mobilising insights from professionals across disciplines, this session will highlight the need for new governance models that acknowledge the benefits of involving multidisciplinary stakeholders – including laboratory medicine – in organisational decision-making to successfully address complex healthcare challenges and drive healthcare transformation.
SPEAKERS:
- Prof John Dillon, Professor of Hepatology and Gastroenterology, University of Dundee
- Dr Ellie Dow, Consultant in Biochemical Medicine, NHS Tayside
- Prof. Federico Lega, Professor in Healthcare Management at Department of Biomedical Sciences for Health, University of Milan
Moderated by Dr. Colleen Strain, Scientific Manager, Scientific Leadership and Education, Core Diagnostics, Abbott
This session is hosted by the UNIVANTS of Healthcare Excellence Award and Abbott. The UNIVANTS of Healthcare Excellence program is a prestigious global award that was created by Abbott in partnership with leading healthcare organisations with a common vision to inspire and celebrate healthcare excellence. The UNIVANTS of Healthcare Excellence Award recognises teams who collaborate across disciplines and transform healthcare delivery, and ultimately patients lives. The UNIVANTS of Healthcare Excellence Award celebrates clinical care teams that unify for greater outcomes. Previous winners have led best practices that demonstrate the powerful benefits of laboratory insights combined with interdisciplinary clinical care.


 Towards a new hospital model based on innovation and knowledge transfer
Towards a new hospital model based on innovation and knowledge transfer
More information on this session coming soon.
This session is hosted by INTERREG – INNHOSPITAL.

Connect with participants and explore the exhibition area
 Ageing and health: the politics of better policies
Ageing and health: the politics of better policies
Longer lives are a triumph in human history. Yet many observers regard ageing populations as a problem, in large part due to the costs of caring for older people. For these observers, the success of twentieth-century public policy in expanding longevity contains the seeds of a crisis for twenty-first-century social policy. This belief in the inevitability of an age-related fiscal crisis often coincides with a belief in the inevitability of intergenerational conflict over public spending priorities.
Fortunately, these beliefs are incorrect. In fact, there is not much evidence that population ageing irreparably imperils health systems, economies, or societies. Why then, do so many policymakers act like it does?
In this session, based on new book from the European Observatory on Health Systems and Policies and published by Cambridge University Press entitled “Ageing and health: the politics of better policies” we dismantle conventional wisdom on the economic, societal and political consequences of population ageing and consider what it takes to get lifecourse policies in place that benefit people of all ages.
Most of the problems ascribed to inequality between generations (intergenerational equity) are actually a result of inequality within society as a whole that spans across age groups (intragenerational equity). Policies that address these broader inequalities are also often the best for addressing the specific needs of older or younger people. These policies are built on the life-course perspective, which focuses on identifying the policies which can make people happier and healthier at all ages by drawing on the context and circumstances under which aging occurs. It is possible to construct coalitions of politicians and interests that can develop and support sophisticated life-course policies that lessen the burdens of ageing and health on everybody. Rather than focusing on – or creating – conflict between generations over scarce resources, life-course policies which improve the health and productivity of people at all ages are more effective ways to produce health, equity, and economic sustainability.
The takeaway message is that intergenerational inequality is not, and need not be, a significant problem. It is substantially a product of current and past intragenerational inequality, and in fact inequality between generations often goes with inequality within generations. Intergenerational conflict is a distraction from policies that promote greater equality within and between generations – talk of an ageing crisis is frequently just another version of longstanding arguments against public social investment from cradle to grave.
Speakers:
- Prof Scott L. Greer, Professor of Health Management and Policy, University of Michigan, USA
- Ass. Prof Aaron Reeves, Associate Professor, University of Oxford, United Kingdom
- Dr Michelle Falkenbach, Postdoctoral Associate, Cornell University, USA
- Prof Jane Gingrich, Professor of Comparative Political Economy, University of Oxford, United Kingdom
- Dr Jonathan Cylus, Head of London hubs, European Observatory on Health Systems and Policies, United Kingdom
- Prof. Minakshi Raj, Assistant Professor, University of Illinois at Urbana-Champaign
This session is hosted by the European Observatory on Health Systems and Policies. The Observatory is a partnership that brings together different policy perspectives to identify what health systems and policies evidence Europe’s decision makers need. The Observatory then generates and shares the evidence in print, in ‘person’ and on-line – acting as a knowledge broker and bridging the gap between academia and practice.
 ABSTRACT SESSION on Sustainability of health services
ABSTRACT SESSION on Sustainability of health services
Human health is closely intertwined with environmental sustainability. A case in point is the growing care needs arising from climate change and emerging diseases. At the same time, the healthcare industry is responsible for a non-negligible part of the global greenhouse gas emissions. The use of environmentally friendly practices and service delivery is therefore urgently needed.
The following abstracts will be presented:
- SustHealthv2: evidence-informed assessment tool for sustainable high-quality healthcare buildings
Dr Andrea Brambilla, Politecnico di Milano, Department ABC, Design & Health Lab, Italy - Train healthcare professionals for an environmental sustainability of health services
Dr Estelle Baures, EHESP, France - Management of pharmaceutical waste: The practices and perception (example from Serbia)
Dr Milica Paut Kusturica, Research Associate at Faculty of Medicine, PhD, Pharmacoeconomics Specialist, University of Novi Sad, Serbia - Climate Pact Ambassador role in the decarbonisation of healthcare sector
Dr Marija Jevtic, MD PhD, full professor Faculty of Medicine University of Novi Sad, EUPHA ENV, Climate Pact Ambassador
Moderated by Prof. Susana Viegas, Escola Nacional de Saude Publica
 ABSTRACT SESSION on Integration of care for community-living patients
ABSTRACT SESSION on Integration of care for community-living patients
In recent years, health systems around the world have been moving towards integrated, patient-centered care in an effort to avoid a fragmented delivery of care. Numerous benefits arise from providing comprehensive care services, including better patient experience, improved health outcomes and quality of care, and financial efficiency. This abstract session will highlight the different ways in which integrated care has been implemented in various settings.
The following abstracts will be presented:
- Untangling the interrelatedness within integrated care programmes for community-dwelling frail older people: a rapid realist review
Dr Anam Ahmed, Panaxea, The Netherlands; Radboud University Medical Centre, The Netherlands - Exploring the factors causing discontinuity of chronic care
Ms Anu Vehkamäki, Aalto University, Finland - Towards platform solutions in care coordination – Identifying occurrences of fragmentation in Parkinson’s Disease care
Ms Annika Bengts, HEMA Institute, Department of Industrial Engineering and Management, Aalto University School of Science, Finland - Reforming care for people with (multiple) chronic conditions: what matters to them?
Prof Mieke Rijken, Nivel, The Netherlands; University of Eastern Finland, Finland - From design to practice: People powered integrated health
Ms Katerina Tarasova, Health Assessment Europe, Belgium; Accreditation Canada, Canada - Navigator: On-line clientship profiling helps to tailor integrated care
Ms Riikka Riihimies, Clinical Instructor, Tampere University, Tampere, Finland; Valkeakoski Health Center, Valkeakoski, Finland
Moderated by Prof. Adalberto C. Fernandes, Escola Nacional de Saude Publica, Portugal
 EHMA PIE: Governance and leadership
EHMA PIE: Governance and leadership
EHMA PIE is a space for discussions that are Provocative, Innovative and
Encouraging (PIE) and can help shape the future of health management. Through EHMA PIE, we aim to address complex topics, spark provocative discussions, and foster connections across the entire health ecosystem.
The following idea will be presented:
- Pandemic Preparedness: what position do the methods in policy surveillance and legal epidemiology have in the legislation provision for future public health pandemic?
Sharmi Haque BSc(Hons), Bachelor Medicine & Master Medicine Student, Master Governance and Leadership in European Public Health Student, Bachelor (Hons) Clinical Sciences, Faculty of Health, Medicine and Life Sciences, University of Maastricht
SOCIAL EVENT: Book launch & drinks
Everything you always wanted to know about EU health policy…and COVID-19 responses
The EU institutional and changes brought about as a response to the pandemic a substantial and far reaching. EU health policy has often been overlooked and was never on the political agenda. COVID-19 and the pandemic response, however, changed this dramatically. EU-health policy has become centre stage followed by bold investments and new regulatory initiatives. Obvious examples are the EU4Heatlth programme, the Recovery and Resilience fund, the new agency HERA, the new remit for the European Medicines Agency and the European Center for Disease Control. There are also new European Commission mechanisms with regards to the purchase of personal protective equipment, supplies, medicines including vaccines and medical technologies.
Building a European Health Union is a bold attempt to put health not only higher on the political agenda but also provide additional mandates, funds and programmes. It will clearly contribute to stronger crisis preparedness and crisis response for Europe. What it means, however, for countries in terms of developing the health systems and public health services is still less clear. Will the EU’s new role in health support reforms in countries such as the strengthening of primary and integrated care? Will it support better accessibility to high quality services? Will it help to strengthen the resilience of health systems? What will it bring for health managers in regional and local authorities, sickness funds, public health offices and primary care centers?
The session is building on the COVID-19 update (forthcoming Oct 2021) of a previously published book on EU-health policy (1st edition 2014, update 2nd edition 2019). In this meet-the-authors session we will discuss with you the major health related changes of the COVID-19 response. This includes the implications for the health mandate and actions for health. We will also discuss implications for the other policies that are health relevant, like workforce, digital or environment. And course the new rules of economic governance of the EU with a view to investment in health and health systems will be central.
Keynote:
- Prof Scott Greer, University of Michigan, USA
Panelists to take your questions:
- Dr Sarah Rozenblum, University of Michigan, USA
- Dr Ellie Brooks, University of Edinburgh, United Kingdom
- Dr Holly Jarman, University of Michigan, USA
- Dr Anniek de Ruijter, Law Centre for Health and Life and University of Amsterdam, The Netherlands
Facilitated by Dr Matthias Wismar, European Observatory on Health Systems and Policies, Belgium
This session is hosted by the European Observatory on Health Systems and Policies. The Observatory is a partnership that brings together different policy perspectives to identify what health systems and policies evidence Europe’s decision makers need. The Observatory then generates and shares the evidence in print, in ‘person’ and on-line – acting as a knowledge broker and bridging the gap between academia and practice.
Day 3 – Friday, 17 September 2021
Health systems resilience during COVID-19: what have we learned?
Health systems resilience can be understood as the health systems’ ability to maintain or improve its performance in the face of a shock, so that the ultimate health systems goals, especially that of improving health of the population, can be achieved. In this session we attempt to summarise key strategies that enabled health systems in Europe to respond resiliently to the COVID-19 pandemic. We grouped these strategies according to the core health system functions, and this session will focus on the financing, resource generation, and service delivery functions. For each of these functions, we will illustrate practical examples of resilience and discuss what we can learn from the national experiences so far for post pandemic recovery and preparedness for future shocks. We will close by drawing attention to the key role of health systems and broader governance, underpinned by strong state capacity, political leadership, and community engagement, in responding resiliently to major shocks such as COVID-19.
This session draws on the study by the European Observatory on Health Systems and Policies “Health systems resilience during COVID-19: Lessons for building back better” and on the content compiled in the COVID-19 Health System Response Monitor (HSRM), which tracks policy responses to the pandemic in the WHO European Region.
SPEAKERS:
- Dr Josep Figueras, Director, European Observatory on Health Systems and Policies
- Dr Erica Richardson, Research Fellow, European Observatory on Health Systems and Policies
- Anna Sagan, Research Fellow, European Observatory on Health Systems and Policies
- Erin Webb, Research Fellow, Technical University of Berlin
- Ruth Waitzberg, Research Fellow, European Observatory on Health Systems and Policies
- Gemma Williams, Research Fellow, European Observatory on Health Systems and Policies
This session is hosted by the European Observatory on Health Systems and Policies. The Observatory is a partnership that brings together different policy perspectives to identify what health systems and policies evidence Europe’s decision makers need. The Observatory then generates and shares the evidence in print, in ‘person’ and on-line – acting as a knowledge broker and bridging the gap between academia and practice.
 ABSTRACT SESSION on Responding to healthcare crisis
ABSTRACT SESSION on Responding to healthcare crisis
Since its onset, the COVID-19 pandemic has had far-reaching impacts on the delivery of care, access to care, management of patients, and overall healthcare systems. In this abstract session, speakers will present some of the responses that were implemented to face the COVID-19 pandemic and mitigate its impacts.
The following abstracts will be presented:
- The innovative drugs economic impact in the management of COVID-19 hospitalised patients
Dr Lucrezia Ferrario, Health Care Datascience Lab, Centre for Health Economics, Social and Health Care Management, Carlo Cattaneo – LIUC University, Italy - COVID-19 as a driver for change: Hospital Outpatient Pharmacy Proximity (HOPP) Program @ CHULC (Centro Hospitalar Universitário Lisboa Central)
Ms Raquel Chantre, Centro Hospitalar Universitário Lisboa Central, Portugal - Adherence to COVID-19 prevention measures and willingness to vaccinate in Greek adults: the role of Health Literacy
Ass Prof Vassiliki Costarelli, Harokopio University, Department of Economics & Sustainable Development, Greece - Gender disparities in access to healthcare during the COVID-19 pandemic: Evidence from the SHARE COVID-19 survey for the aged 50+ population in Europe
Dr Rui Dang, Westminster International University in Tashkent, Uzbekistan - What happened to hospitalisations due to ACSC in Portugal before and after the crisis?
Mr João Victor Rocha, Researcher at National School of Public Health (Portugal); PhD Candidate at NOVA University of Lisbon and Linköping University
Moderated by Prof Dr Kim Putters, Director, Social and Cultural Planning Office, The Netherlands
 ABSTRACT SESSION on Inter-organisational collaboration
ABSTRACT SESSION on Inter-organisational collaboration
Inter-organisational collaboration is increasingly prevalent across healthcare organisations and implies healthcare provision across organisational borders by actors who have a common goal. While it is thought that inter-organisational collaboration have the ability to address wicked health problems and improve the quality of service provision through resource sharing, the effectiveness of such collaborations is still under researched. This abstract session will therefore shed light on the use and impact of inter-organisational collaborations within the healthcare sector.
The following abstracts will be presented:
- How, why, and when do inter-organisational collaborations in healthcare improve performance? A realist evaluation
Dr Justin Aunger, University of Birmingham, United Kingdom - Inter-organisational networks: rational behavior or institutional myths?
MSc Robin Peeters, Department of Health Services Research, Maastricht University, The Netherlands - Career anchors of the physician leaders
Dr Tiina Tuononen, University of Eastern Finland, Finland - Leaders’ and employees’ perceptions on remote leadership in a health and social service organisation
Prof Johanna Lammintakanen, University of Eastern Finland, Finland - Health management: Organisational and individual determinants of the outcomes in hospital context
Prof Tania Gaspar, Lisbon Lusiada University/CLISSIS/COMEGI; ISAMB/Lisbon University, Portugal
Moderated by Dr Ann Mahon, Professor of Health Leadership and Head of the Health Management Group at the University of Manchester
 EHMA PIE: Person Centeredness and Care Integration
EHMA PIE: Person Centeredness and Care Integration
EHMA PIE is a space for discussions that are Provocative, Innovative and
Encouraging (PIE) and can help shape the future of health management. Through EHMA PIE, we aim to address complex topics, spark provocative discussions, and foster connections across the entire health ecosystem.
The following ideas will be presented:
- Transition of care consultation
Ms. Cláudia Teresa Nelas Dias De Almeida - Patient Journey maps – useful tool or gimmick?
Dr Axel Kaehne, Reader Health Services Research, Medical School, Edge Hill University
Connect with participants and explore the exhibition area
 The Recovery & Resilience Facility: a driver of Europe’s ambitions for a resilient Health Union and global health leadership?
The Recovery & Resilience Facility: a driver of Europe’s ambitions for a resilient Health Union and global health leadership?
Through the European Recovery & Resilience Facility (RRF), the European Union will invest €672.5 billion to support investments and reforms across the EU in 6 sectors: green and digital transition; smart and sustainable growth; policies for the next generation; health; and resilience. Allocations per country have been made and, in April Member States submitted their national plans for the use of the Recovery & Resilience Facility. These will be approved over the summer by the European Commission and the European Council. From Autumn 2021, the execution of these plans will begin.
This session aims to provide an overview of the RRF investment plans in the healthcare sector and discuss how implementation of countries’ national plans can become a driver of Europe’s ambitions for a resilient Health Union and global health leadership. Stakeholders from the European Institutions, academia, citizens, and the private sector will share their perspective on how to ensure an efficient implementation of the recovery plans.
SPEAKERS:
- Ms Maria Teresa Fabregas Fernandez, Director – Recovery and Resilience Task Force
- Dr Josep Figueras, Director at the European Observatory on Health Systems and Policies
- Prof. Francesco Saverio Mennini, Centre for Economics and International Studies-Economic Evaluation and Health Technology Assessment, University of Rome
- Dr François Sandre, Head of Europe region for Sanofi Pasteur
- Dr Mariano Votta, Director, Active Citizenship Network / Cittadinanzattiva
Moderated by Ms Caroline Costongs, Director, EuroHealthNet
This session is hosted by Sanofi.
 Build Back Better. Time to act: the burden of cardiovascular diseases
Build Back Better. Time to act: the burden of cardiovascular diseases
COVID-19 has thrust health and patient outcomes into a global spotlight. Organisations and systems needs to define and think differently about going forward – at population and/or patient levels. With appropriate political vision, leadership, commitment to science and innovation, we can continue to grow life expectancy but increase it equitably.
EFPIA and PwC recently published the report Health Systems after COVID-19 that gives eight practical recommendations that are key for European stakeholders to pursue going forward, in partnership. In a nutshell, the recommendations focus on preserving population health sustainably via a shift towards prevention and early care, which can be achieved by e.g. upgrading care practice and healthcare professional training, leveraging technology, and using data to improve outcomes.
For EHMA and Novartis the need to Build Back Better to prevent the emergence of silent pandemics, by learning from the COVID-19 response to tackle existing and future health challenges, is clear. We stand ready, to collaborate and support the Global Community to move along, like discussed, at B20-G20 Dialogue organized under the G20 Italian presidency.
We would like to call all stakeholders and movements from the EU to discuss and looking for ways to “build back better”. Better resilience, better preparedness, better outcomes, are big opportunities for all.
- Better resilience: By optimising care, we will be better prepared to overcome – means we would proactively respond to shocks and structural changes, returning to optimal performance.
- Better preparedness: By ensuring that healthcare systems are fit for purpose by adapting to needs and representing the interests of all.
- Better outcomes: By looking beyond responding to crises and creating systems, which thrive to such an extent, the crises do not derail our progress: transformation results-driven, and implemented for the long-term.
Besides focusing on how we build back better, we also need to act on repercussions of the pandemic on cardiovascular mortality and morbidity risk being exponential unless bold action is taken. Improving cardiovascular health will have a crucial impact on the resilience of our healthcare systems. The digital transformation and the European Health Data Space offer great opportunities to pool patient data across Europe for research and for improving cardiovascular disease prevention, management and delivery of care, like defended by MEP Hearts Group.
Today we are seeing how a pandemic can turn into a Syndemic or secondary pandemic, when health systems do not properly treat a disease for a year due to lack of early detection of disease, diagnosis, and access to treatments, needs. A comprehensive EU policy response to address the increasing burden of cardiovascular disease (CDV) and ensure that citizens can live longer, healthier lives is needed – regardless of where they are born or live in the EU – and enable them to continue to contribute to society and the economy.
Without decisive action starting today, the number of citizens suffering from CVD and the burden of dealing with the disease will increase dramatically. This should be a cause of great concern for policymakers’ prioritization, considering both population health and the effect on health systems, as defended by different organizations that represent; all active players of cardiovascular care: from the to the clinicians and health professionals to research organizations, and management healthcare.
A collaborative solution needs to mobilize research and innovation in CVD (and its interaction with other chronic diseases) and promote public private partnerships in CVD innovation. By leveraging the various policy and funding instruments, including Horizon Europe, the EU4Health Programme, the European Health Data Space and Next Generation EU, as well as through horizontal healthcare and life sciences related policy instruments.
Looking into the future, the projected number of people living with stroke will increase by 35% (from nine million in 2017 to 12 million in 2040). Today cardiovascular disease has been costing to the EU EUR 210 billion per year, due to direct healthcare costs, productivity loss, and informal care by caregivers. In addition, COVID-19 pandemic has been an additional challenge, due to the significant impact it has had on CVD patients, in terms of access to and delivery of care, as well as of heart health and cardiovascular complications.
This is why Collaborative Solutions are so important and needed. Looking beyond the COVID-19 pandemic, there is a need to act on the structural needs. Although recognizing the remarkable progress, societies face persistent challenges. Accordingly, there is a need to ensure that timely access to innovation and care and which benefits both to patients and health systems.
Inspired by the Portuguese Council Conclusions of 2021, that calls for a dialogue to be facilitate among all: Member States, patients and consumers, health professionals, industry and academia in the pharmaceutical and medical device areas, to closely collaborate and to co-create and facilitate solutions – this will be the time to act.
Speakers:
- Dr Birgit Beger, CEO, EU Heart Network
- Ms Maria da Graça Carvalho, Co-Chair of the Heart Group, and Member of European Parliament, Portugal
- Dr Filipe Macedo, Director of Portuguese National CVD Program
- Ms Donata Meroni, Head of Unit – ‘Health promotion and disease prevention, funding’, DG SANTE
- Prof. Fausto Pinto, President, World Heart Federation
- Dr. Janneke Van der Kamp, Region Europe Head, Novartis Pharmaceuticals
Moderated by Dr Alexandre Lourenço, President, Associação Portuguesa de Administradores Hospitalares (APAH).
This session is hosted by Novartis. Novartis purpose is to reimagine medicine to improve and extend people’s lives. They use innovative science and technology to address some of society’s most challenging healthcare issues. They discover and develop breakthrough treatments and find new ways to deliver them to as many people as possible. They also aim to reward those who invest their money, time and ideas in our company.
Connect with participants and explore the exhibition area
 POSTER PRESENTATIONS
POSTER PRESENTATIONS
In this pitching session authors will present their posters. Posters will remain available in the exhibition area for the entire duration of the Conference. You can contact the authors via the Conference platform for any questions or more information.
In this session the following posters will be presented:
Under the sub-theme ‘Person-centeredness and care integration’
- Examining specific leadership competencies of medical social workers, used in managing child protection cases within multi-disciplinary teams in a children’s hospital by Ms Sheila Mc Crory
- Four meta-theoretical ways to view integrated care by Dr Anneli Hujala
- Scirocco Exchange Knowledge Transfer Programme for Capacity-building in Integrated Care by Ms Birgit Sandu Gociu
- Home palliative care costs by Mr João André Santos
- Delineating the type 2 diabetes population in the Netherlands using an all-payer claims database: specialist care, medication utilization and expenditures 2016–2018 by MSc Rose Geurten
- Patient or “Homo Consumer”: how changes in the Institutional logics change the healthcare system by Ms Anna Wohlthat
- Hospital at home in Portugal the first five years: numbers, figures and patterns by Dr Joana Faro
- The demand for urgent care services in Portugal by Dr Patrícia Alves Rocha
Under the sub-theme Improving healthcare access and outcomes
- The Pediatric Orthopedics workforce in Romania and its impact on clubfoot patients’ access to health care services by Ms Bianca Duran
- Primary care teams: dynamics after COVID by Dr Antoni Peris Grao
Under the sub-theme ‘Managing the digital transformation’
- Digital & Innovation Skills Helix in health – The DISH project by Ms Sabine Paasch Olsen
 The WHO framework and partnership working
The WHO framework and partnership working
The NHS is in the process of flipping the script and working towards a completely new way of working – really bringing together partnerships across health and social care. The World Health Organization (WHO) have also put out a framework about partnership working, principles and standards which align with the NHS approach.
During this session we will be exploring the mindset of change, led by Jacque Mallender from Economics by design who will talk through the WHO standards and principles and how these can be applied both in the UK and across Europe.
Speakers:
- Jacque Mallender, Economics By Design
- Stephen McCulloch, Director of Communications, Good Governance Institute
- Lena Samuels, Chair, South Central Ambulance Service NHS
Foundation Trust; Chair, Hampshire and IOW ICS, South East Regional People Board, Council of the Association of Ambulance Chief Executives; Independent Chair, Hampshire and Isle of Wight ICS.
Moderated by Prof Andrew Corbett-Nolan, CEO, Good Governance Institute
This session is hosted by the Good Governance Institute (GGI). GGI is an internationally respected consultancy and knowledge institute working across the UK. They help organisations create a fairer, better world by improving how they are led and governed.
 ABSTRACT SESSION on Operations management, logistics and procurement
ABSTRACT SESSION on Operations management, logistics and procurement
Effective operations management, logistics and procurement are key to reduce waste of time and resources, mitigate the inflation of healthcare costs, and ensure the availability of supplies. This session will explore the benefits of joint purchasing, the implementation of lean management, the decision-making processes behind procurement, and the introduction of appointment systems.
The following abstracts will be presented:
- Collaborating within a bad marriage: the case of joint purchasing of expensive medicine
Dr Bart Noort, University of Groningen, The Netherlands - Making Lean Management initiatives last: identifying barriers and facilitators towards Lean Management sustainability
Dr Oskar Roemeling, University of Groningen, The Netherlands - Decision-making processes for Magnetic Resonance Imaging technology procurement: decision-makers perspectives
Dr Maria Maia, Institute for Technology Assessment and Systemsnalysis (ITAS), Karlsruhe Institute of Technology (KIT), Germany. Interdisciplinary Centre of Social Sciences (CICS.NOVA), NOVA School of Science and Technology (FCT NOVA), Portugal - Implementing a flexible outpatient appointment system in presence of distinct urgency-based blocks
Dr Chiara Morlotti, University of Bergamo, Italy
Moderated by Ms Hayley Welsh, Senior Consultant at Optimat Ltd
 ABSTRACT SESSION on Improving healthcare outcomes
ABSTRACT SESSION on Improving healthcare outcomes
A core theme of health management is the improvement of healthcare outcomes. This session will dive into the different ways healthcare outcomes can be ameliorated, including through efficiency improvement, quality development, organisational management, home hospitalisation, and reduce in-hospital stay amongst other.
The following abstracts will be presented:
- Quality development of multidisciplinary team meetings in oncological care including patients’ perspectives in treatment decisions: an overview
MMag Andrea Schweiger, Karl Landsteiner Institute for Hospital Organization, Vienna, Austria; University of Klagenfurt, Klagenfurt, Austria - Defining delayed discharges of inpatients and their impact in acute hospital care: a scoping review
Mr Alexander Micallef, University of Malta, Malta - Hospital at home versus hospital care in patients with the main diagnosis of influenza and pneumonia
Dr Joana Faro, Centro Hospitalar Tondela Viseu, EPE, Portugal - Strategic upgrading for efficiency improvement: the preoperative checklist in the protocol “femoral neck fracture in patients over 65 years” at the UOC of Orthopaedics and Traumatology – University Hospital of Verona
Dr Jacopo Fagherazzi, Università degli Studi di Verona, Italy
 EHMA PIE: Managing the digital transformation
EHMA PIE: Managing the digital transformation
EHMA PIE is a space for discussions that are Provocative, Innovative and
Encouraging (PIE) and can help shape the future of health management. Through EHMA PIE, we aim to address complex topics, spark provocative discussions, and foster connections across the entire health ecosystem.
The following ideas will be presented:
- Linking blockchain and environmental sustainability in healthcare management
Dr Rui Dang, Senior Lecturer in Health Economics at Westminster International University in Tashkent and Visiting Professor in Demographic Economics at Gdansk University of Technology - The European Collaborative Action on Medication Errors and Traceability patient safety project
Ms Laura Cigolot, Head of Secretariat, European Alliance for Access to Safe Medicines (EAASM)
Moderated by Ass Prof Dr Eva Turk, University of Oslo, Norway; University of Maribor, Slovenia
Connect with participants and explore the exhibition area
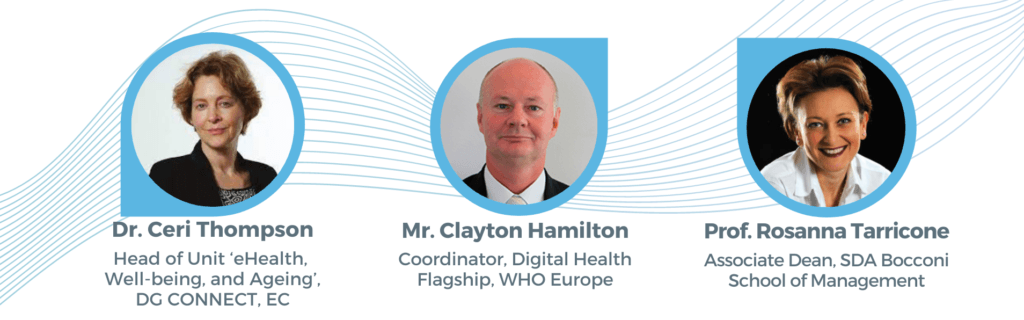
 Digital transformation in healthcare: digital technology as a management tool
Digital transformation in healthcare: digital technology as a management tool
The digitalisation of healthcare is an essential enabler to transforming the delivery of care and improving patient experience. The critical role of digitalisation and the need to drive the digital transformation of health systems have become even more evident during the COVID-19 pandemic, when digital technologies have been deployed in unprecedented ways to support the provision of essential care services. Beyond the delivery of services, digital technologies are being used as a management tool that impacts both the organisation of work and staff well-being.
What innovative solutions can health and care organisations deploy to increase the sustainability of healthcare? How is digital technology being used as a management tool? What is the impact of health data on decision-making at the managerial level?
Keynote:
- Dr Ceri Thompson, Deputy Head of Unit ‘eHealth, Well-being, and Ageing’ in the Directorate General for Communications Networks, Content and Technology (DG CONNECT) of the European Commission
Panelists:
- Mr Clayton Hamilton, Coordinator, Digital Health Flagship, Division of Country Health Policies and Systems, World Health Organization (WHO) Europe
- Prof Rosanna Tarricone, Associate Dean, SDA Bocconi School of Management
Moderated by Dr Alexandre Lourenço, President, Associação Portuguesa de Administradores Hospitalares (APAH) and Master of Ceremonies of EHMA 2021
Closing Ceremony
Award Ceremony
- Karolinska Medical Management Center (MMC) & EHMA Research Award
This Award was established to stimulate early career researchers to engage in healthcare management research. At its 18th edition, the Award will recognise the best doctoral thesis in the field of health management. - EHMA Awards for best European Paper, best non-European Paper, and Best Poster
Closing remarks by:
- Dr Axel Kaehne, President, European Health Management Association (EHMA)
Moderated by Dr Alexandre Lourenço, President, Associação Portuguesa de Administradores Hospitalares (APAH) and Master of Ceremonies of EHMA 2021





